
Mum-of-one Lisa Parker was just 47 when she died at the Hospice in July 2017 after being diagnosed with motor neurone disease two-and-a-half years earlier.
Her MND had become so complicated that her husband Ant says he doesn’t know how they would have coped without the Hospice and since her death, he describes it as his ‘safe haven’ of support that he and their 11-year-old son Zack look forward to coming back to.
Here, Ant shares their story...
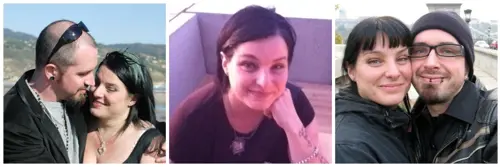
Lisa and I met in the late 90’s through our work in the film industry in creature and make-up effects - she as a fabricator, puppet maker and costume-maker and me as a sculptor, painter and prosthetic make-up artist.
For nearly 10 years, as good friends, we shared many interests and inspirations and I’d admired her attractive personality and kind, caring nature from afar, but in September 2007, while we were working on a movie project in Budapest, we finally got together. A month later we were already talking about families and in December 2008, our beloved son Zack was born.
We worked together on our own art too, making characters using both of our skills, displaying them through a Berlin gallery that represented us and showing and selling them at galleries, art fairs and conventions across Europe and America.
We’d juggle our work schedules so one of us was always at home with Zack or occasionally even take him with us, even living in Germany for six months at one point while I was working on a movie filming in Berlin and doing some work for the gallery while we were there.
It was a wonderful time being able to do all that together as a family. In December 2011 we got married on Malibu Beach in the beautiful sunshine, while our little boy played in the sand. It felt like life couldn’t get much better.

But during the summer of 2014, Lisa developed a limp, started tripping up a lot and losing the strength in an increasingly painful wrist. She saw her GP who thought she was suffering from arthritis in her leg and carpal tunnel syndrome in her wrist. But no sooner had she started treatment than it became clear she was suffering from foot drop too, which led to her GP thinking that her symptoms might be connected to a neurological disorder.
She was referred to a neurologist and a series of grueling and invasive tests began, including lumbar puncture and electromyography (EMG), which uses needles to record the nerve impulses within muscles. The second EMG test lasted a whole hour and it was this that gave the diagnosis.
As I heard the neurologist, who’d sent my wife for some of the most torturous tests, say ‘It’s not good news,’ everything went still and seemed to stop for a moment.
Despite all the anticipation in the world about what words could possibly follow, nothing could have prepared us for the diagnosis. ‘You have a rare condition called Motor Neurone Disease. I’m afraid there is no cure.’ Everything stopped again.
The date – 26th January 2015 - will remain etched on my soul. That day the whole world fell out of our little family and everything changed forever.
I’d heard of MND. Only a few months earlier Facebook had been full of videos of people taking the ALS (Amyotrophic Lateral Sclerosis – another term for MND) Ice Bucket Challenge, but little did we know that Lisa was already suffering the symptoms of the same devastating disease.
Like most, I only really knew of MND as the disease that Professor Stephen Hawking suffered from - a neurodegenerative disease that causes increasing disability and eventually death. He beat the odds, surviving from his early 20’s into his 70’s, but the average life expectancy is usually just 2 - 5 years.
We were told the disease would find its own pace, affecting different people in different ways and it’s the truest thing we were ever told.
From the start, Lisa’s condition gradually declined until it reached sudden drop-offs where her base-line would drastically drop like a stone, sometimes in a matter of days.
So from walking with a limp to walking with a stick, she’d be walking with a walker. From having to use a wheelchair and being able to transfer herself onto a chair or bed, she’d be having to transfer from a wheelchair with help, to relying on being hoisted.
In March 2016, the disease started affecting her lungs and her breathing. Worried she was in danger of respiratory and cardiac arrest, her respiratory doctors started her on a ventilator that she used at night. At the same time, the muscles in her mouth and throat began to weaken, affecting her ability to swallow.
To pre-empt a time when she couldn’t eat, she was fitted with a RIG (Radiologically Inserted Gastrostomy) – a special feeding tube into her stomach, but it wasn’t long before she started having serious issues with her swallowing and speech, relying more and more on the feeding tube.
In May 2016, we moved into an open plan house in Chesham, by which time Lisa was using a big motorised wheelchair all the time. We had a special vehicle with a ramp. She needed a profiling bed. We knew a hoist was next.
Over the summer, while Lisa was in hospital due to problems with her feeding tube, she passed an assessment for NHS Continuing Health Care and carers started coming in to help wash, dress and help with her greatly increasing care needs, that were becoming too much for me to handle myself and look after a small child. I don’t think I have to tell you how distressing and frustrating it was for a 46-year-old to have to rely on someone to dress her and take care of her most personal hygiene.
The hardest part was watching Lisa have everything taken from her. We always knew it was going to take her life but before it did, it was going to take everything else first. To watch her daily struggle as her body literally gave up on her day by day was horrendous, heart-breaking and painful and having a child watch that too was sometimes just too much.
I knew that Christmas 2016 would be our last one together, so I cancelled as many carer visits as I could and managed all her medication and care myself. That way there were no strangers, as Zack called them, in our home and we could just be the three of us in our own private space.
Putting Lisa’s Christmas dinner - such a symbolically special meal and one that Lisa loved - into a blender and turning it into a puree so she could manage to swallow it was a real low point for me - even to this day, it’s a difficult memory.
In the New Year, a nurse who used to visit us from Rennie Grove, saw how much we were all struggling. There were a lot of complications and issues with Lisa’s care that were affecting all of us so in February 2017, Lisa was transferred by ambulance from St Thomas’ Hospital in London where she’d been having respiratory care, to The Hospice of St Francis in the hope that they could get on top of some of her symptoms. She was losing weight fast because of muscle wastage and having problems with her feeding tube, which by then, she relied on all the time.
After two weeks at the Hospice, she didn’t want to leave and the Hospice made her feel comfortable enough to make that choice - to sacrifice being at home, around her child all the time because she knew it would be better for us all. That was Lisa - always thinking about what would be best for everyone else. It was a turning point. Looking back, I honestly don’t know how we’d have coped any other way.
Although I greatly appreciate and admire the work of health and social care professionals, our experience had shown that knowledge and education are seriously lacking in how best to support MND sufferers and their families, leading to a lot of avoidable stress and distress.
But the Hospice medical team worked so hard to get it right - to understand how best to support Lisa, a very strong woman who knew her own mind and how she wanted things done; to win her and my trust; to work together to deal with the challenge of her profoundly complex needs, and to respond and adapt to them as they changed on a daily basis.

So that we could spend precious family time together comfortably, they gave us one of two double rooms available and were always respectful of our privacy. They took time to get to know Lisa as a person and what mattered to her. Zack got to know the people who were looking after his mum so they were no longer strangers and it became normal to him and I was able to continue to help with Lisa’s care - it was very important to me to be able to help look after my wife.
While I was there, the nurses knew that I’d take care of Lisa’s feeds and fluids through her feeding tube. I’d drop Zack off at school and make my way over to the Hospice to be with Lisa until it was time to pick Zack up. We’d come back together most days after school and spend the weekends there too. We even had film nights together some weekends. The Hospice gave us the space to have the much-needed quality family time that by then, we weren’t even able to get at home.
Lisa was able to enjoy reflexology and Jacuzzi baths to relax and calm her and every small detail made such a difference – whether it was one of the nurses giving Zack fish food so he could feed the tadpoles in the pond as he watched the dragonflies or Kate and Claire, the nurses Lisa had a special rapport with, dyeing her hair black when her roots began to show.
One month at the Hospice soon became three, and by June this awful disease had robbed her of pretty much everything, including her ability to speak, meaning she relied on a computer screen, controlled with her eye movements, to communicate. Even with that, they had all the time and patience in the world.
They cared, it’s quite simple - they just cared. No matter how hard it was, the Hospice was so supporting and comforting – a total home away from home.
Right at the end, I’d been here a few nights with Lisa by myself while a friend looked after Zack. I’d never imagined him being at the Hospice at the end, but this friend suggested I bring his PlayStation up. We connected it to Lisa’s TV in her room and he sat in this big comfy chair playing Minecraft.
Lisa was pretty much asleep by that point but I knew she knew we were there. I remember sitting there in her room with my eyes closed, listening to the music and sounds from Zack’s Minecraft game and for a minute, it felt like we were all back at home. In the most unbelievable of circumstances and given what was about to happen, it just felt like everyone, including Lisa, was at peace for the first time in a long time. Zack and I both stayed that night, Zack sleeping in a bed beside her. I didn’t really sleep and that night turned out to be her last – she died the next morning with Zack and myself and her mum and sister with her.
Claire, one of the nurses who was closest to Lisa, came in, even though it was her day off, to wash Lisa and make her look nice, which meant a lot to us all and while this was happening, Jo, a senior nurse who keeps horses, went and got Kimmie her little grey pony, who Zack knew from the Hospice’s Pony Days we’d been to, and led Zack out to her.
It was such a profoundly beautiful moment – this little boy who had been totally and understandably silent in the moments after losing his mum, just got onto little Kimmie and crumpled. ‘I feel sad,’ he said, wrapping his arms around her neck. For him to have that release, just walking around the garden on that early July morning, helped so much.
For all of us but for Zack especially, the support has been beyond words. He’s been to most of the Children’s Pony Days, which are held each month between March and September and where children facing loss are led round the beautiful gardens and woodland on Jo’s horses and pony by her and her team of young volunteers.
We’ve come to half term children’s activities, Saturday Family Film Mornings and a Children’s Gymkhana and he likes coming back - it helps us to build positive memories and he finds it all very calming and reassuring.
Since six weeks after Lisa died, I’ve received regular calls from the Hospice’s Bereavement Support Line volunteers asking me how I’m doing but it wasn’t until April 2018, nine months later, that I started having 1:1 bereavement support with Lesley, one of the Hospice’s bereavement counsellors.
I knew it was the right time and that I needed it and if I’m getting the help I need, it’s easier for me to have strategies in place to help Zack. Lesley’s support has been amazing – she’s someone who cares enough to maybe not understand everything, but to hear it.
I look forward to coming to the Hospice because it’s a reason to be here. I want to be here because when I am, even though it makes me think back to the last difficult months of Lisa’s life, it’s a place where strangely, I still feel quite close to her, which makes me feel comfortable and safe.
I don’t find it easy to talk about things but it feels good on lots of different levels. Our lives have changed completely and it’s not easy being a single parent. I don’t have much support around and for most of the time, it’s just Zack and I but I try to carry on working around him as best I can.
I don’t feel calm or comforted or relaxed a lot of the time but I do when I come here. It’s become our safe haven and I feel like that because of how much being here meant to Lisa and to all of us.
You can’t help but think if things had been different what would we be doing now? Where would we be? So having someone to share those thoughts and feelings with in a place like this is wonderful.
Even in the darkest moments, the Pony Days gave Zack a little ray of light and as he’s grown physically and moved from Kimmie the pony to horses like Alfie and Max, to me they feel like symbols of his journey and his growing confidence.
I can’t begin to imagine what life would have been like had Lisa stayed at home without this place and without its care and I want to share our story so that in some small way, I can give something back.”






Share Article